12 State Perspectives on Essential Changes During COVID-19
Takeaways from the Delta Center Convening #5
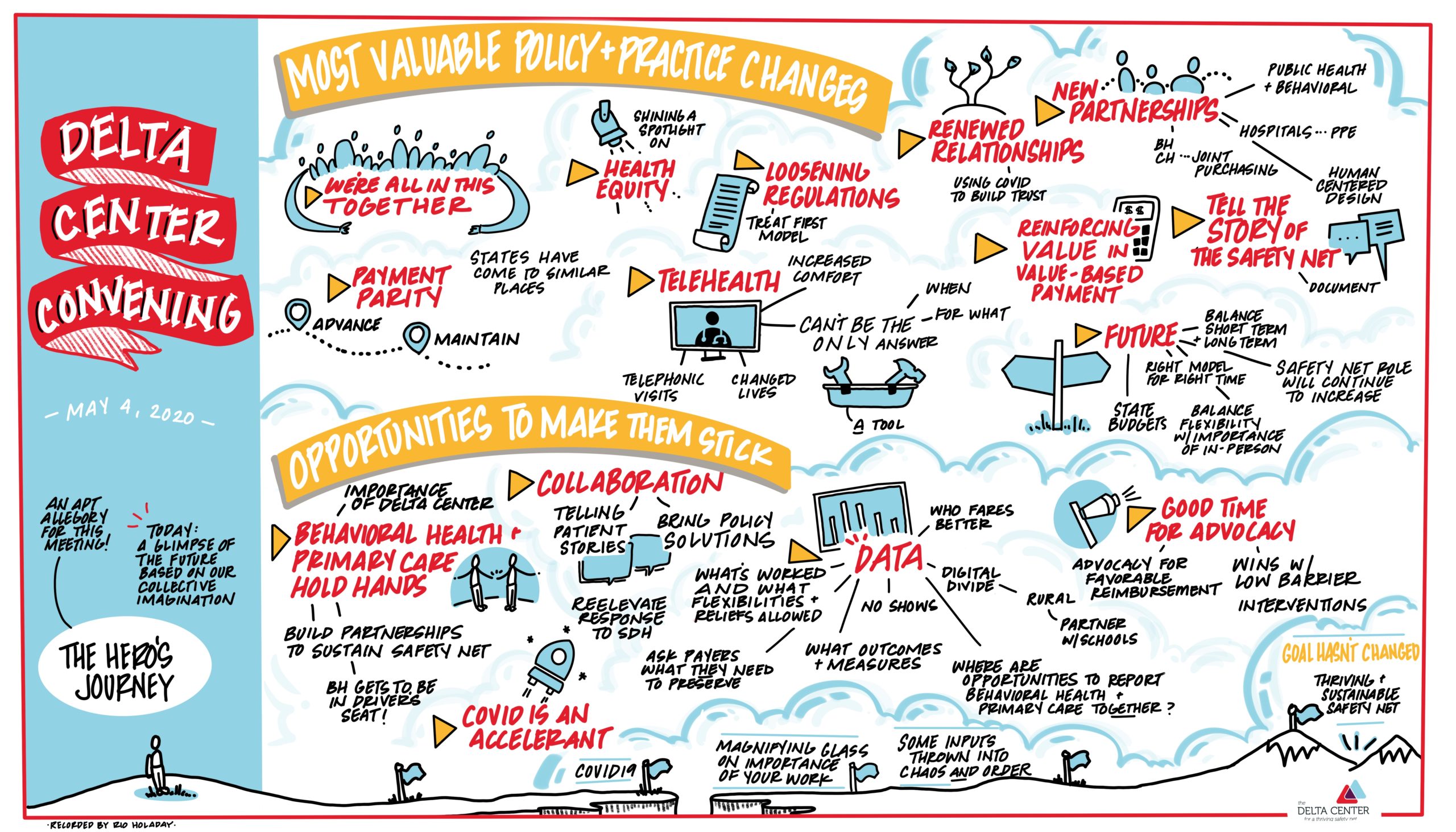
Image: Thank you to Rio Holaday for capturing our convening meeting with this beautiful illustration!
The Delta Center for a Thriving Safety Net held a virtual convening on May 4, 2020. Like so many others, the Delta Center’s path has been altered by COVID-19, but the ultimate goal of building and supporting a unified, thriving, and financially sustainable safety net remains and is more important than ever. Participants from the twelve Delta Center states reflected that looking ahead, they share a new challenge: the economic fallout of the pandemic means that states will simultaneously face increased demand for safety-net services and shrinking funds to address these needs.
Rachel Tobey, co-director of the Delta Center, framed the convening with the idea that, like in the classic “hero’s journey,” the world will be transformed from here forward, and it is imperative that we intentionally shape what emerges.
The COVID-19 crisis has underscored the important work that associations are doing through the Delta Center, building partnerships between primary care (PC) and behavioral health (BH), understanding which policy levers serve mutual goals, and creating opportunities to work together on what’s next. Delta Center grantees discussed positive changes in policy and care that were newly implemented or accelerated due to COVID-19. They also began to brainstorm the actions—particularly collective actions by PC and BH—that would be needed for these changes to stay in place going forward.
Below, we highlight the main themes of the small group and panel discussions.
In the classic hero’s journey—the archetypal plot structure of myths and movies—the protagonist reluctantly departs from normal life, enters the unknown, endures successive trials, and eventually returns home, having been transformed…If such a character exists in the coronavirus story, it is not an individual, but the entire modern world. The end of its journey and the nature of its final transformation will arise from our collective imagination and action…
– Ed Yong, The Atlantic
What are the most valuable POLICY changes you or your members have made that has impacted patients and/or consumers?
- Prospective payment: It is clear that prospective payment can be a lifeline for organizations facing massive and sudden decreases in face-to-face visits. Health centers in Oregon and Washington operating under capitation-like alternative payment models were able to nimbly respond to the crisis in ways that other providers were not. Even though behavioral health providers have historically not received prospective payments, Oregon’s behavioral health state association managed to secure a lump sum prospective payment for non-Medicaid behavioral health services as part of the emergency response, a critical move for ensuring stability of the care system. State associations are observing the natural experiment of this pandemic and asking whether members engaged in value-based payment models have fared better than their counterparts whose revenue comes predominantly through fee-for-service payments.
- Telehealth reimbursement policy: Increased flexibility in reimbursement, including reimbursement for telephonic and video visits, has been critical to maintaining access to care during the pandemic and has made telehealth a more financially sound solution than ever before, at least in the short term. While some providers were already conducting telehealth visits, this shift in state payment policy accelerated adoption of telehealth services among PC and BH providers and patients/consumers. Many states reported that no-show rates for tele-behavioral health services in particular were exceptionally low. Both PC and BH state associations were very interested in keeping payment for telehealth as a strategy for expanding access to care in the medium- and long-term. States also reported a range of experiences with telehealth reimbursement rates. In New Mexico, state associations were able to make a direct request to their Medicaid director to make sure that telephonic and video visits were reimbursed at health centers’ full PPS rate, whereas New York reported challenges with telehealth visits being reimbursed at significantly lower rates. PCAs also highlighted the financial challenge of Medicare paying less for telehealth than for an in-person health center visit.
What are the most valuable PRACTICE changes you or your members have made that has impacted patients and/or consumers?
- Major shift to telehealth: The dramatic shift to telehealth comprising the majority of visits for behavioral health and primary care providers is going a long way to bridge the gap in care and is also creating new access opportunities. However, state associations also expressed concern about inequities in telehealth, especially in the divide for those who are able to have video visits and those who can use telephonic visits only. It is still an outstanding question whether video, in particular, is an equitable solution given broadband and technology concerns. Communities have rapidly innovated in response to these challenges. For example, in rural Maine, health centers handed out tablets as a solution and school districts across the country are experimenting with school bus wifi hotspots. However, associations cautioned that while telehealth is a great tool, it doesn’t meet the needs of all ages or all conditions, and that providers will need to consider how to bridge gaps in access and quality of care.
- Regulatory loosening: Several regulations have been loosened in the face of the crisis and have advanced access to care in ways that behavioral health providers have been requesting for some time. This has included fewer burdensome assessments prior to engaging clients in behavioral health therapy, a treat-first model allowing care to be provided prior to a diagnosis, and increased information sharing between primary care and substance use disorder providers due to waiving restrictions around 42 CFR. Other changes have included allowing more autonomous care to be delivered by more of the healthcare workforce (e.g., decreased supervision of nurse practitioners).
What opportunities exist for PC and BH to facilitate making these policy and practice changes stick?
- Measurement and data: Strong measurement and data will help associations and their members advocate for continued flexibilities in regulations (e.g., licensure, telehealth payment parity) that have allowed them to deliver care that meets the needs of the individuals and families they serve. It is important that associations and their members not only document flexibilities, but point specifically to which regulatory flexibilities allowed them to make the changes that resulted in improved access and/or higher quality care for patients/consumers. COVID-19 and the ensuing mental and physical health needs will also present a critical opportunity to look at where PC and BH can jointly measure outcomes to continue to make the case for the effectiveness and necessity of integrated care. Grantees from multiple states highlighted that this may require thinking “beyond HEDIS” in terms of how safety-net providers are delivering value to the care system. Data on patient satisfaction through surveys or data on utilization of telehealth services will help to tell the story of the safety net in this critical time. Looking forward, state associations also discussed asking payers directly what evidence of impact they will need in order to retain relaxed regulations or other interim policy changes that have led to positive outcomes.
- Telling the story of the safety net: COVID-19 has underscored the importance of financial stability in the safety net. The current crisis and the visibility of health care and public health presents an opportunity for PC and BH to advocate for payment policy that supports better care and greater flexibility. Associations emphasized that a key tool will be telling the story of the safety net, including lifting up consumer voices.
Without this grant I don’t think that conversation would be as likely – the dialogue and communication between us is far better than it’s ever been. I feel comfortable to ask them [counterpart association] anything. In thinking about the future, and future crises like this, it opens my mind to what’s possible with community partners that we often didn’t think about.
– Delta Center Grantee
- Partnerships: Strong partnerships, such as those forged over the course of the Delta Center, will be critical for the safety net to quickly and efficiently respond to patient and consumer needs going forward. COVID-19 has both accelerated and challenged partnerships—between PC and BH and between safety-net providers and managed care organizations (MCOs), the State, and community-based organizations. Some partnerships are facilitating critical connections needed to meet the social needs of patients and consumers during this period of economic instability. They have also already helped associations and their members to partner to meet immediate needs such as procurement of PPE and testing. COVID-19 is also creating new challenges for state Medicaid agencies, MCOs, and associations as states face impending budget shortfalls paired with projected increases in enrollment and a wave of mental health needs that will put pressure on already strained and under-resourced behavioral health care systems. Some reflected that in times of scarcity, there can be an inclination to retreat from collaboration while others emphasized that times like this demand that PC and BH see themselves as partners as much as ever.
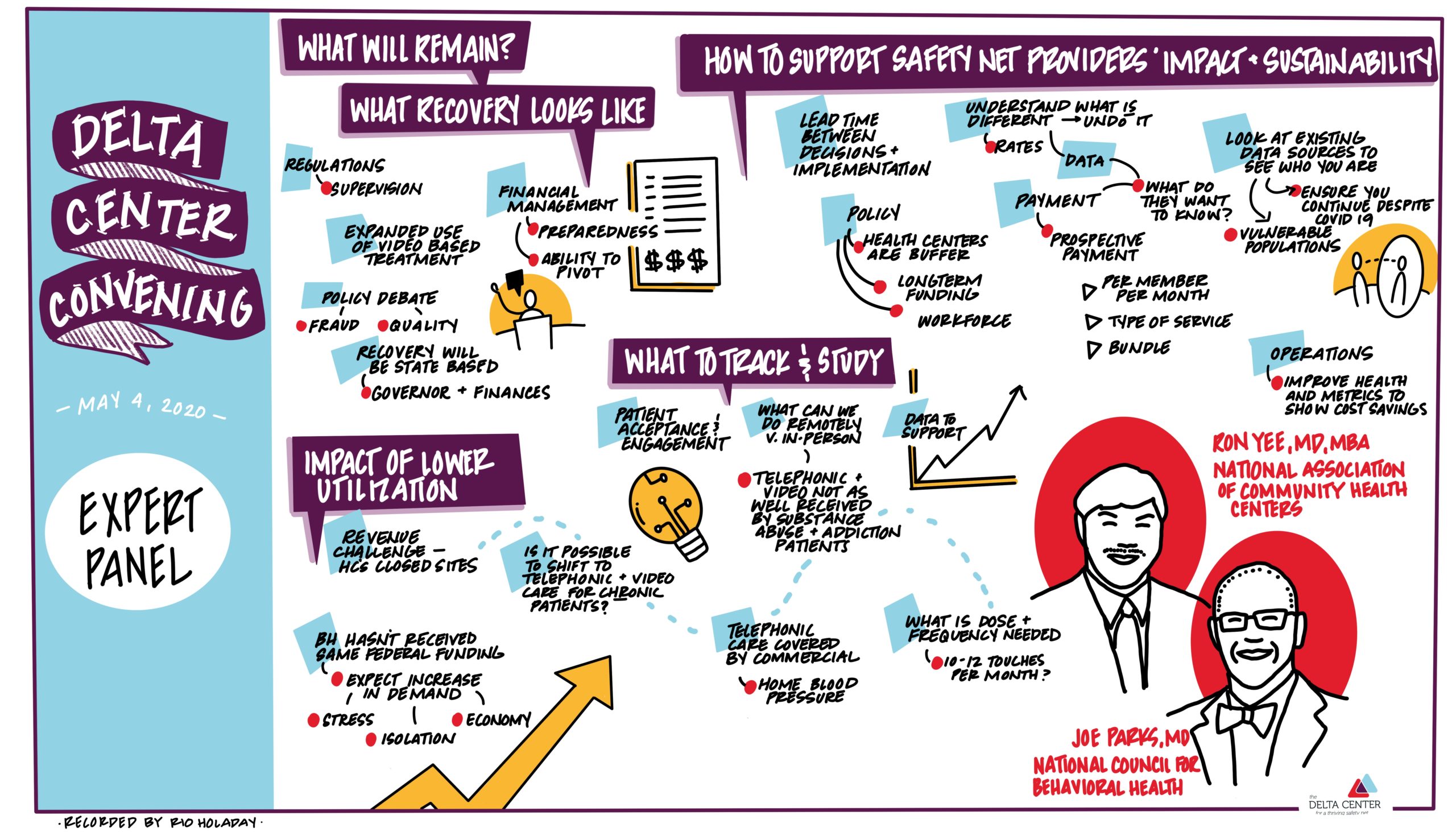
We ended the meeting with an expert panel featuring Joe Parks, M.D., Medical Director, from the National Council for Behavioral Health, and Ron Yee, MD, MBA, FAAFP, Chief Medical Officer of the National Association of Community Health Centers. (See illustration below by Rio Holaday)